- Multidisciplinary treatment with immune checkpoint inhibitors for advanced stage hepatocellular carcinoma
-
Ahlim Lee, Jaejun Lee, Hyun Yang, Soo-Yoon Sung, Chang Ho Jeon, Su Ho Kim, Moon Hyung Choi, Young Joon Lee, Ho Jong Chun, Si Hyun Bae
-
J Liver Cancer. 2022;22(1):75-83. Published online March 18, 2022
-
DOI: https://doi.org/10.17998/jlc.2022.03.04
-
-
3,972
Views
-
93
Downloads
-
3
Citations
-
 Abstract Abstract
 PDF PDF
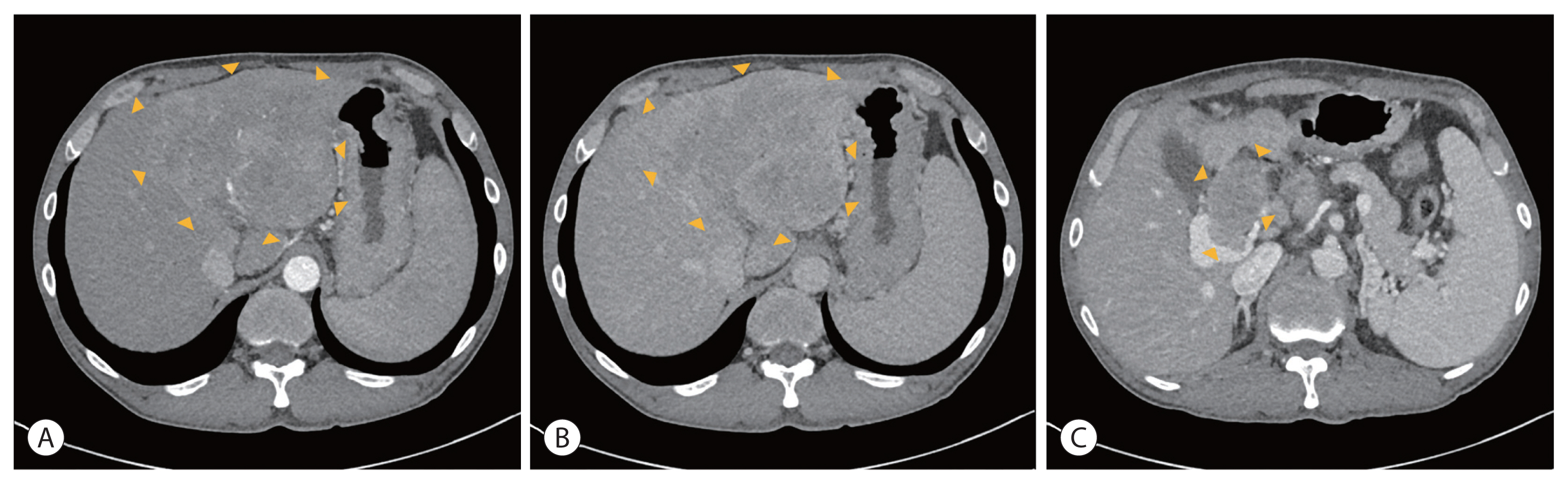
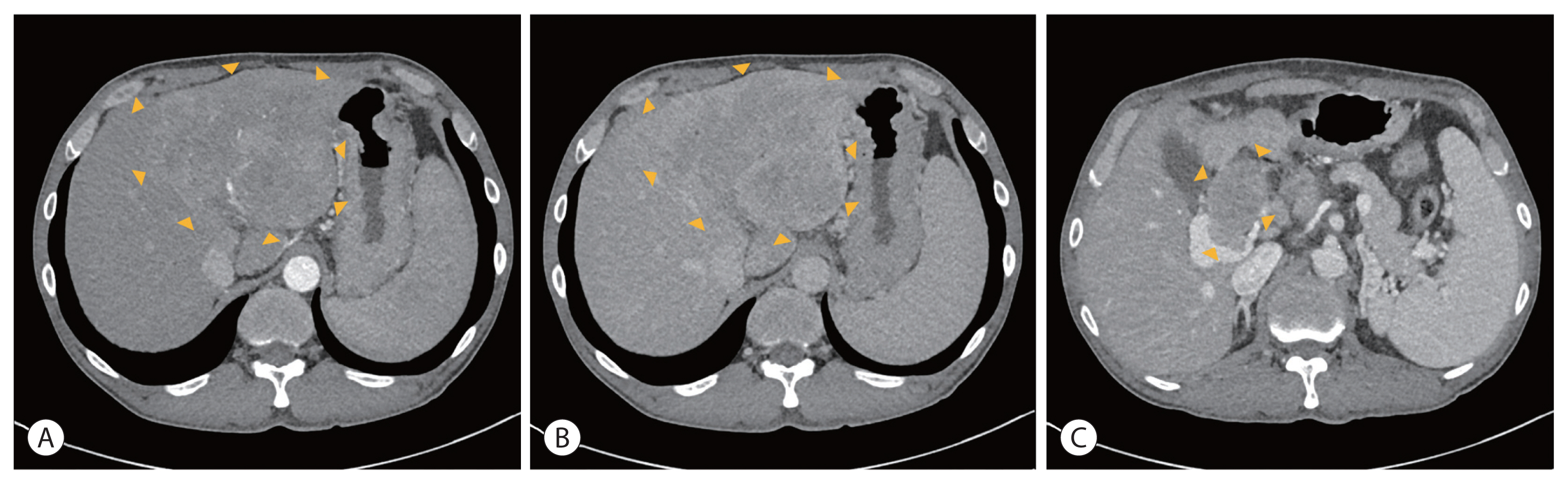
- Hepatocellular carcinoma (HCC) is a cytotoxic chemotherapy-resistant tumor and most HCCs arise in a background of liver cirrhosis of various causes. Although the IMBrave150 trial showed remarkable advancements in the treatment of unresectable HCC with atezolizumab plus bevacizumab (AteBeva), therapeutic outcomes were unsatisfactory in more than half of the patients. Accordingly, many ongoing trials combine conventional modalities with new drugs such as immune checkpoint inhibitors for better treatment outcomes, and they are expected to benefit patients with limited responses to conventional treatment. Here, two patients with advanced stage HCC with preserved liver function and good performance status showed partial response after treatment with combination or sequential therapy of AteBeva, hepatic arterial infusion chemotherapy, radiation therapy, and transarterial chemoembolization. These findings indicate the efficacy of multidisciplinary treatment against advanced HCC. Additional studies are required to establish optimal treatment strategies.
-
Citations
Citations to this article as recorded by  - Complications of immunotherapy in advanced hepatocellular carcinoma
Young-Gi Song, Jeong-Ju Yoo, Sang Gyune Kim, Young Seok Kim
Journal of Liver Cancer.2024; 24(1): 9. CrossRef - Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab
Tae Hyun Kim, Bo Hyun Kim, Yu Ri Cho, Young-Hwan Koh, Joong-Won Park
Journal of Liver Cancer.2023; 23(2): 330. CrossRef - Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
Won Hyeok Choe
Journal of Liver Cancer.2022; 22(1): 1. CrossRef
- Infiltration of T Cells and Programmed Cell Death Ligand 1-expressing Macrophages as a Potential Predictor of Lenvatinib Response in Hepatocellular Carcinoma
-
Pil Soo Sung, Sung Woo Cho, Jaejun Lee, Hyun Yang, Jeong Won Jang, Si Hyun Bae, Jong Young Choi, Seung Kew Yoon
-
J Liver Cancer. 2020;20(2):128-134. Published online September 30, 2020
-
DOI: https://doi.org/10.17998/jlc.20.2.128
-
-
3,274
Views
-
98
Downloads
-
6
Citations
-
 Abstract Abstract
 PDF PDF
- Background/Aim
s: Lenvatinib was recently proven to be non-inferior to sorafenib in treating unresectable hepatocellular carcinoma (HCC) in a phase-3 randomized controlled trial. In this study, we investigated whether the response to lenvatinib was affected by tumor immunogenicity.
Methods
Between May 2019 and April 2020, nine patients with intermediate-to-advanced HCC, who were treated with lenvatinib after liver biopsy, were enrolled. Immunohistochemical staining and multi-color flow cytometry were performed on specimens obtained from liver biopsy.
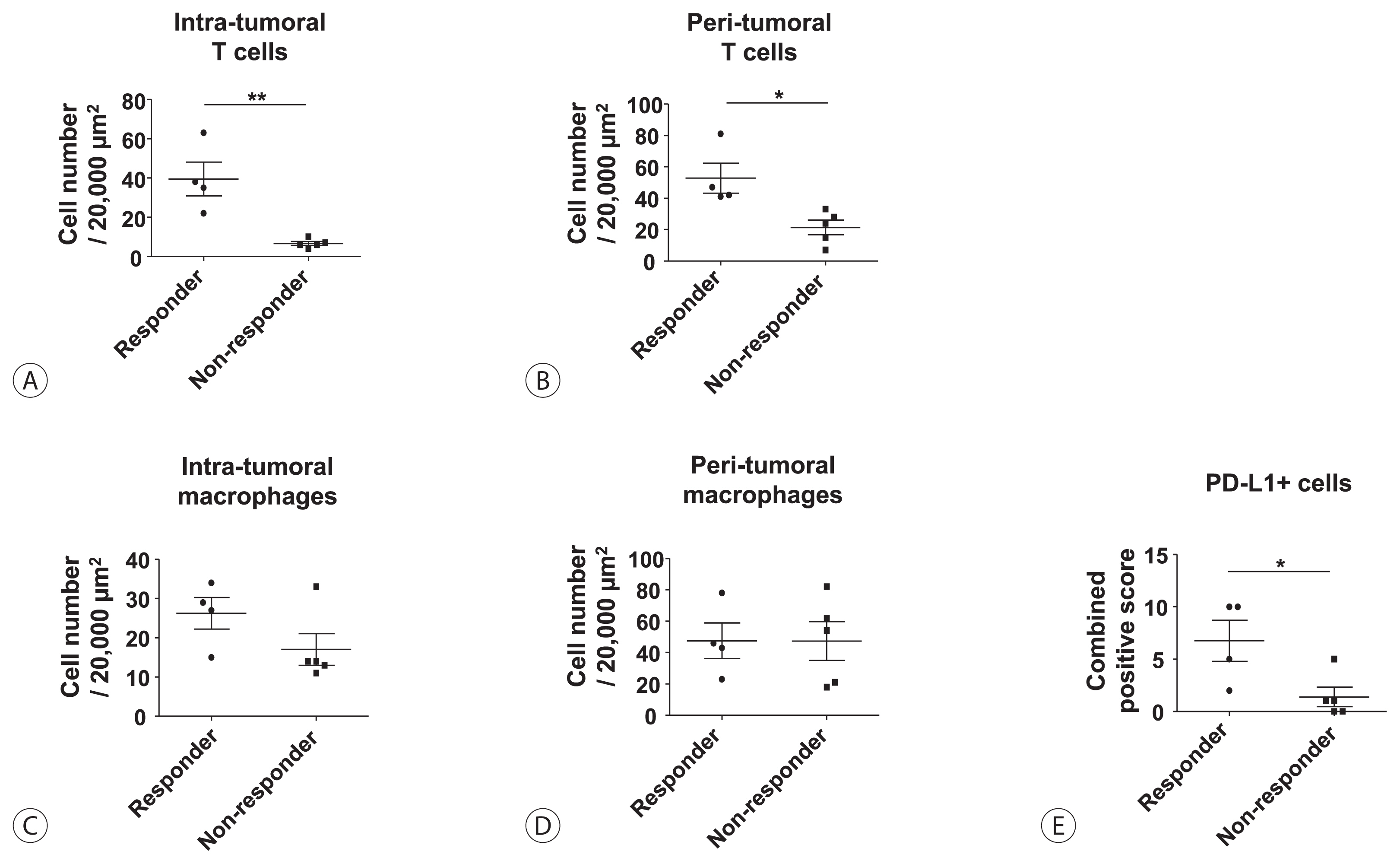
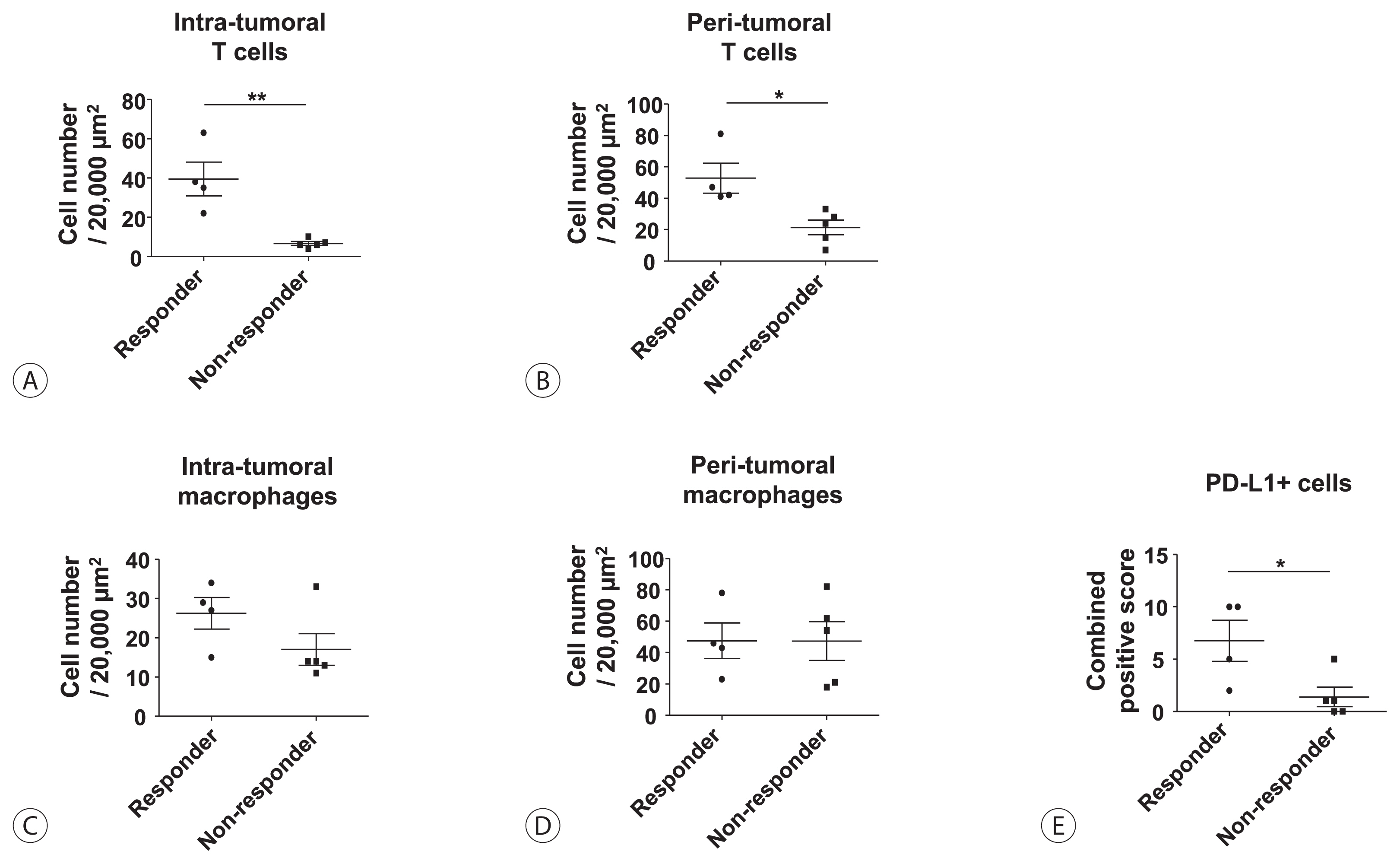
Results
Among the nine patients enrolled, four showed objective responses (complete responses+partial responses). Immunohistochemical staining for CD3, CD68, and programmed cell death ligand 1 (PD-L1) demonstrated that patients with objective responses showed marked infiltration of T cells and PD-L1-expressing macrophages in intra-tumoral and peri-tumoral tissues compared to those without objective responses. A significant difference in the numbers of infiltrated T cells, both in the intra-tumoral (P<0.01) and peri-tumoral regions (P<0.05), were identified between responders and non-responders. Regarding the number of infiltrated macrophages, no significant difference was found between the responders and non-responders, although the number of PD-L1-expressing tumor-associated macrophages was significantly higher in responders than that in non-responders (P<0.05).
Conclusions
Tumor immunogenicity, as indicated by T cell and PD-L1-positive macrophage infiltration, affects lenvatinib response in unresectable HCC.
-
Citations
Citations to this article as recorded by  - Higher Number of Tumor-Infiltrating PD-L1+ Cells Is Related to Better Response to Multikinase Inhibitors in Hepatocellular Carcinoma
Ji Won Han, Ji Hoon Kim, Dong Hyun Kim, Jeong Won Jang, Si Hyun Bae, Jong Young Choi, Seung Kew Yoon, Jaegyoon Ahn, Hyun Yang, Pil Soo Sung
Diagnostics.2023; 13(8): 1453. CrossRef - Intrahepatic inflammatory IgA+PD-L1high monocytes in hepatocellular carcinoma development and immunotherapy
Pil Soo Sung, Dong Jun Park, Pu Reun Roh, Kyoung Do Mun, Sung Woo Cho, Gil Won Lee, Eun Sun Jung, Sung Hak Lee, Jeong Won Jang, Si Hyun Bae, Jong Young Choi, Jonghwan Choi, Jaegyoon Ahn, Seung Kew Yoon
Journal for ImmunoTherapy of Cancer.2022; 10(5): e003618. CrossRef - Crosstalk between tumor-associated macrophages and neighboring cells in hepatocellular carcinoma
Pil Soo Sung
Clinical and Molecular Hepatology.2022; 28(3): 333. CrossRef - Blood-based biomarkers for immune-based therapy in advanced HCC: Promising but a long way to go
Pil Soo Sung, Isaac Kise Lee, Pu Reun Roh, Min Woo Kang, Jaegyoon Ahn, Seung Kew Yoon
Frontiers in Oncology.2022;[Epub] CrossRef - Immunological Mechanisms for Hepatocellular Carcinoma Risk after Direct-Acting Antiviral Treatment of Hepatitis C Virus Infection
Pil Soo Sung, Eui-Cheol Shin
Journal of Clinical Medicine.2021; 10(2): 221. CrossRef - Preferential Expression of Programmed Death Ligand 1 Protein in Tumor-Associated Macrophages and Its Potential Role in Immunotherapy for Hepatocellular Carcinoma
Dong-Jun Park, Pil-Soo Sung, Gil-Won Lee, Sung-Woo Cho, Sung-Min Kim, Byung-Yoon Kang, Won-Hee Hur, Hyun Yang, Soon-Kyu Lee, Sung-Hak Lee, Eun-Sun Jung, Chang-Ho Seo, Joseph Ahn, Ho-Joong Choi, Young-Kyoung You, Jeong-Won Jang, Si-Hyun Bae, Jong-Young Cho
International Journal of Molecular Sciences.2021; 22(9): 4710. CrossRef
- Early Onset Polymorphic Post-transplant Lymphoproliferative Disease Mimicking a Solitary Necrotizing Abscess in a Graft Liver
-
Pil Soo Sung, Jaejun Lee, Joon Lee, Hee Chul Nam, Si Hyun Bae, Seung Kew Yoon
-
J Liver Cancer. 2019;19(2):165-170. Published online September 30, 2019
-
DOI: https://doi.org/10.17998/jlc.19.2.165
-
-
 Abstract Abstract
 PDF PDF
- Although post-transplantation lymphoproliferative disease (PTLD) after liver transplantation is very rare, its prognosis is worse than that of PTLD following other types of solid organ transplantation. Here, we report a rare case of early onset polymorphic PTLD in a graft liver occurring five months after deceased-donor liver transplantation due to hepatocellular carcinoma and hepatitis C virus infection. Initially, findings from contrast-enhanced magnetic resonance imaging mistakenly suspected the lesion was a necrotizing abscess with central necrosis. However, 18F-fluorodeoxyglucose positron emission tomography and biopsy findings confirmed an Epstein-Barr virus (EBV)-associated, B cell type polymorphic PTLD with central necrosis. Our case suggests regular monitoring of EBV serologic status for liver transplant recipients who were initially in an EBV seronegative state. Although early-onset PTLD is very rare after liver transplantation, PTLD should be suspected when recipients show the seroconversion for EBV proteins and the development of new tumors with various clinical presentations.
|